A ray of hope for neglected African disease: sickle cell disease

Sickle cell disease (SCD) is a gene mutation that affects over 300 000 newborn babies every year, nearly three-quarters of those in sub-Saharan Africa. Ninety per cent of babies with SCD in Africa are believed to die before the age of five years. To respond to this disease on the continent, a range of research groups under the leadership of UCT’s Professor Ambroise Wonkam have secured US$3.7 million to establish the Sickle Africa Data Coordinating Center (SADaCC), which will build capacity to help Africa tackle this disease.

Professor Ambroise Wonkam, professor and senior specialist in the Division of Human Genetics at UCT, and the principal investigator for the Sickle Africa Data Coordinating Center (SADaCC).
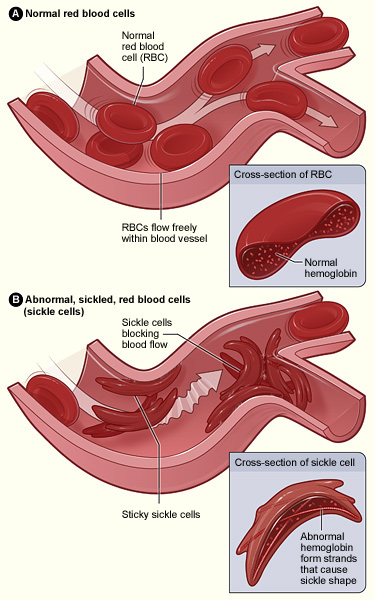
We rely on our red blood cells, specifically the haemoglobin in those cells, to carry oxygen from our lungs to all the tissues of our body. These red blood cells are disc shaped, so they can easily move through both the large and small blood vessels all over the body. But sickle cell disease is a genetic mutation that causes haemoglobin to develop into stiff little rods within the red blood cell. That misshaped haemoglobin forces the red blood cell into a crescent or sickle shape, which hampers its ability to move through blood vessels. These sickle cells cause blockages in the blood vessels, cutting off oxygen supply to critical parts of the body like the organs, brain and eyes.
“Sickle cell disease impacts extremely negatively on the quality of life of a patient,” says Professor Ambroise Wonkam, professor and senior specialist in the Division of Human Genetics in the Faculty of Health Sciences, and principal investigator for SADaCC. “Symptoms of the disease include anaemia (due to the short lifespan of the deformed red blood cells), episodes of severe pain caused by the sickle-shaped red blood cells blocking blood flow in the body, frequent infections, and delayed growth and vision problems as the sickle cells block blood vessels to the eyes.”
The disease is also accompanied by major risk factors – such as pulmonary hypertension (high blood pressure in the lungs), organ damage, stroke, blindness and kidney dysfunctions and failure – that ultimately lead to a short life expectancy, if untreated.
A turning point for SCD?
Despite the high incidence of SCD, there has been little investment in basic research into the disease, specifically in Africa.
“The first case of SCD was described more than 100 years ago, but there is still only one medication (hydroxyurea) available for treatment,” says Wonkam.
His research has been dedicated to remedy this history of neglect. This work has recently paid off with the announcement of the US National Institutes of Health (NIH) and National Heart, Lung and Blood Institute (NHLBI) funding SADaCC.
“The centre will allow us to build a robust platform to support the activities of a companion Pan African Sickle Cell Disease Consortium (SPARCo), which brings together leading SCD researchers and clinicians from high-, middle- and low-income countries to bring about real change – not only for victims of SCD but affected communities and regions.
“The work of SADaCC can be described as that of a conductor of a pan-African sickle research orchestra,” says Wonkam. “The four main activities of the centre include administrative planning and coordination across various sites in Africa, research design and training of field investigators, monitoring and implementation of the research and data management, and analysis and publication of research results.”
Key to the work of SADaCC is the coordination of longitudinal cohort studies. “These are the most scientifically rigorous methods in understanding the risk factors, health and disease outcomes, as well as training and public policy for the disease,” says Wonkam.
“The SADaCC will measure its success not only by research impact in the way we understand both the scientific and clinical aspects of the disease at the scientific and clinical level, but by the way that understanding helps us treat patients effectively. The centre will therefore have a direct impact on how patients are treated in clinics,” he says.
Critical to the future work of SADaCC is the focus on translating the research into policy and practice changes. One of the main conditions of the NIH/NHLBI grant was a formal commitment from the ministries of health in the collaborating countries.
African research for African diseases
Wonkam says it is critical that the research for effective management and treatment for SCD is developed in Africa, as it is Africans who are worst affected.
“The mutation that causes SCD is the same as those that confer a resistance to malaria,” explains Wonkam. “SCD is thus most prevalent in populations living in areas of the world where malaria has been endemic for a long time – and so Africa and its populations are worst affected.”
The mutation is also highly prevalent in the Arabic peninsula and India, and among some people of European descent who have been exposed to malaria for a long time, such as those in the southern parts of Italy and Portugal. Sections of Africa – such as South Africa – that have not been affected by malaria for thousands of years do not experience high levels of the mutation. SCD does, however, affect African Americans, whose genetics still contain the mutation.
“It is important to say that, while more than 70% of SCD patients worldwide live in Africa, most advances in the molecular understanding and management of SCD have been based on research conducted in either the US or the UK,” says Wonkam.
“Clearly contemporary research tools must now be widely implemented in Africa. Therefore, SADaCC has a capacity-building dimension, as the SCD studies will be performed from design, clinical and molecular analysis and reporting, right here on the African continent.”
Story by Natalie Simon.
Image Ambroise Wonkam by Michael Hammond
Image: Cross section sickle cell disease public domain courtesy Wikimedia Commons