Research: Clinical trials of tuberculosis vaccines in the era of increased access to preventive antibiotic treatment

Professor Mark Hatherill, has co-authored: " Clinical trials of tuberculosis vaccines in the era of increased access to preventive antibiotic treatment" appearing in the Lancet Respiratory Medicine.
Abstract:
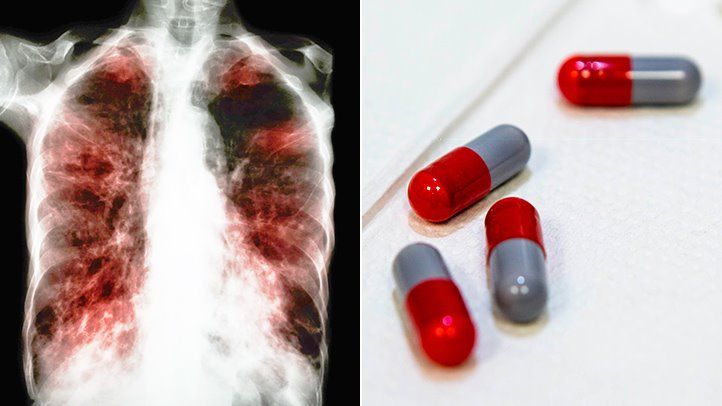
Approximately 10·6 million people worldwide develop tuberculosis each year, representing a failure in epidemic control that is accentuated by the absence of effective vaccines to prevent infection or disease in adolescents and adults. Without effective vaccines, tuberculosis prevention has relied on testing for Mycobacterium tuberculosis infection and treating with antibiotics to prevent progression to tuberculosis disease, known as tuberculosis preventive treatment (TPT). Novel tuberculosis vaccines are in development and phase 3 efficacy trials are imminent. The development of effective, shorter, and safer TPT regimens has broadened the groups eligible for TPT beyond people with HIV and child contacts of people with tuberculosis; future vaccine trials will be undertaken in an era of increased TPT access. Changes in the prevention standard will have implications for tuberculosis vaccine trials of disease prevention, for which safety and sufficient accrual of cases are crucial. In this paper, we examine the urgent need for trials that allow the evaluation of new vaccines and fulfil the ethical duty of researchers to provide TPT. We observe how HIV vaccine trials have incorporated preventive treatment in the form of pre-exposure prophylaxis, propose trial designs that integrate TPT, and summarise considerations for each design in terms of trial validity, efficiency, participant safety, and ethics.
Conclusion
Considering TPT explicitly in trials of novel tuberculosis vaccines has implications for study design, trial efficiency, participant safety, ethics, and human rights responsibilities, and, for some designs, generalisability of trial results. Because of the challenges associated with these considerations, developers might prefer study designs that restrict enrolment to people for whom TPT is not indicated. However, such trials miss an opportunity to generate safety and efficacy data on new tuberculosis vaccines in some of the populations that need them the most. The recent experience of HIV vaccine trials shows that developing trial designs that allow researchers to meet their ethical obligation to provide a standard of prevention, while also retaining the scientific ability to assess the safety and efficacy of novel vaccines, is possible. Simulation studies of the vaccine trial designs proposed in this paper will be important to test the implications of each design on safety, sample size, likely benefit–risk or effect, and therefore cost, as has been done in the HIV vaccine field.
As vaccine developers prepare to initiate phase 2b and phase 3 trials for tuberculosis candidate vaccines, it will be important to define a standard prevention package that is owed to all trial participants or subsets of trial participants, and to articulate the place of TPT within that package. This step should always start with an assumption of TPT eligibility, in line with normative guidance, and place the burden of proof on researchers to justify why TPT can be removed from the standard prevention package in the case of specific groups or circumstances. TPT involves a comprehensive set of linked activities that begin with the identification of people at risk of tuberculosis and the screening for and ruling out of active disease before providing antibiotics to treat tuberculosis infection and prevent progression to active disease. This is the standard of prevention for people in priority risk groups for whom TPT is currently recommended, including people living with HIV and recent contacts of people with tuberculosis. Most importantly, discussions on the standard prevention package should occur in close concert with the individuals and communities affected by tuberculosis that will be asked to host clinical trials of tuberculosis vaccines. The acceptability of and public trust in future tuberculosis vaccines will depend on how decisions about TPT are made together by researchers, funders, and community representatives, and what trade-offs future trial participants are willing to make.
