Research: Protein kinase C-delta (PKCd), a marker of inflammation and tuberculosis disease progression in humans, is important for optimal macrophage killing effector functions and survival in mice

SATVI authors Associate Professor Tom Scriba, Dr Stanley Mbandi Kimbung, Fatoumatta Darboe and Dr Adam Penn-Nicholson have co-authored a paper titled "Protein kinase C-delta (PKCd), a marker of inflammation and tuberculosis disease progression in humans, is important for optimal macrophage killing effector functions and survival in mice" appearing in the Mucosol Immunology Journal.
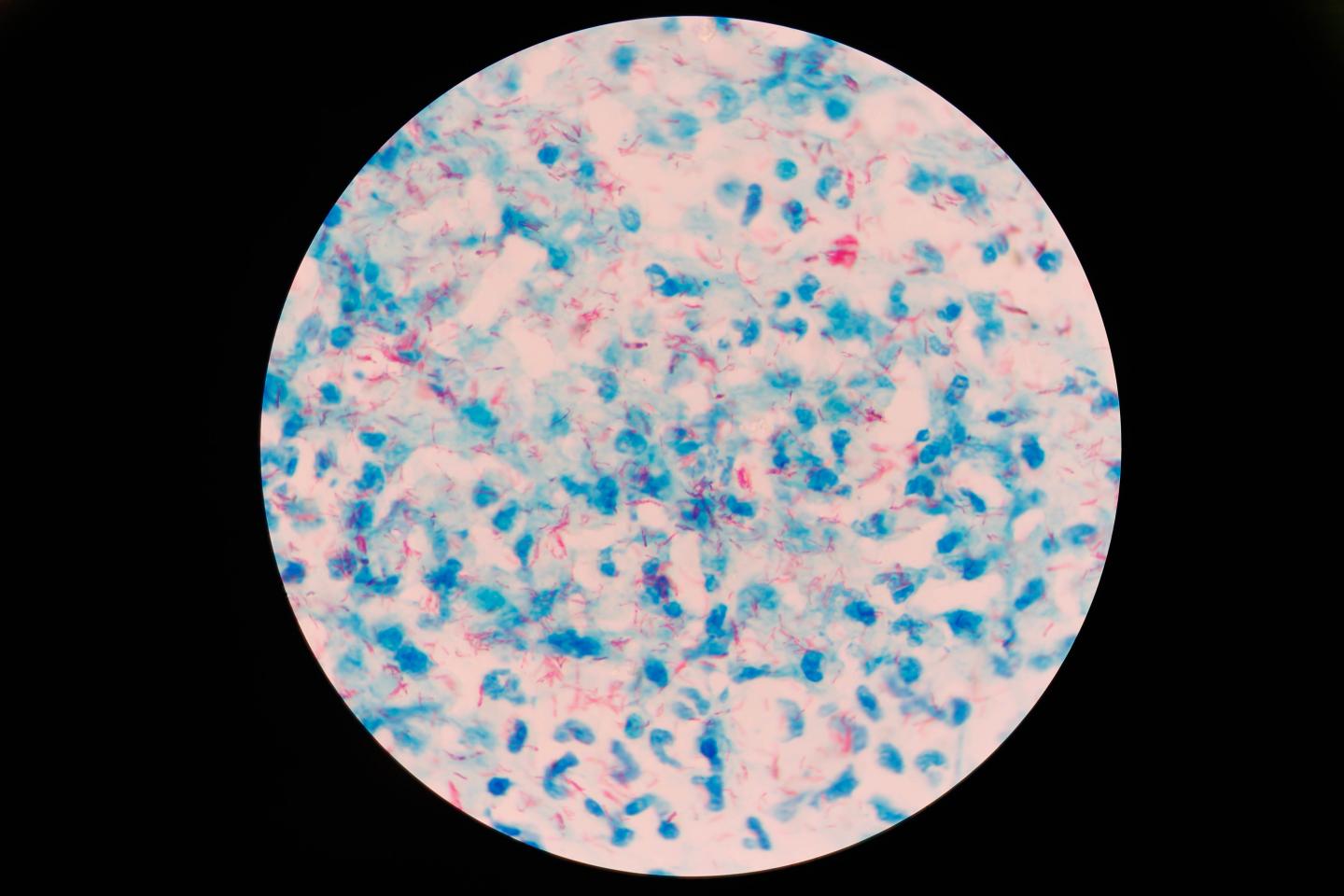
Abstract: We previously demonstrated that protein kinase C-δ (PKCδ) is critical for immunity against Listeria monocytogenes, Leishmania major, and Candida albicans infection in mice. However, the functional relevance of PKCδ during Mycobacterium tuberculosis (Mtb) infection is unknown. PKCδ was significantly upregulated in whole blood of patients with active tuberculosis (TB) disease. Lung proteomics further revealed that PKCδ was highly abundant in the necrotic and cavitory regions of TB granulomas in multidrug-resistant human participants. In murine Mtb infection studies, PKCδ−/− mice were highly susceptible to tuberculosis with increased mortality, weight loss, exacerbated lung pathology, uncontrolled proinflammatory cytokine responses, and increased mycobacterial burdens. Moreover, these mice displayed a significant reduction in alveolar macrophages, dendritic cells, and decreased accumulation of lipid bodies (lungs and macrophages) and serum fatty acids. Furthermore, a peptide inhibitor of PKCδ in wild-type mice mirrored lung inflammation identical to infected PKCδ−/− mice. Mechanistically, increased bacterial growth in macrophages from PKCδ−/− mice was associated with a decline in killing effector functions independent of phagosome maturation and autophagy. Taken together, these data suggest that PKCδ is a marker of inflammation during active TB disease in humans and required for optimal macrophage killing effector functions and host protection during Mtb infection in mice.
We have demonstrated the functional role of PKCδ in host defense against Mtb infection in humans and mice. PKCδ is highly expressed in human whole blood during active TB disease progression as well as within the Mtb-specific proinflammatory regions of necrotic and cavitary lung granulomas during TB disease. These regions of high proinflammatory signatures are required for an early control of bacterial replication and could lead to necrotic damage (caseation) and consequent cavity formation if not appropriately regulated.
Evidently, PKCδ was more abundant in the caseous and cavitary regions in this study, colocalizing with antimicrobial signature and the regions of abundant lipids in granulomas.
However, it is not clear whether mediators of inflammation and antimicrobials are responsible for the overwhelming inflammation at the site of infection, or they are remnants of a robust immune response meant to eliminate the pathogen in the lung. Consistently, we found PKCδ as an indicator of lung inflammation in yet another whole-blood transcriptome data set from pulmonary infections such as sarcoidosis, TB, pneumonia, and lung cancer.
Given the nonspecificity to TB and substantial overlap in PKCδ expression between our cohorts, this kinase offers a limitation to be used as a prognostic marker. Distinctly using mass spectrometry, we showed that the expression of PKCδ varies within the regions of lung granuloma. Notably, anti-TB therapy decreased PKCδ expression in whole blood of human patients, reflecting a potential role for this protein kinase as a host factor regulating Mtb-driven inflammation.
Our findings revealed that PKCδ is indeed associated with host defense against murine TB as PKCδ ablation enhanced mortality with rapid weight loss, high bacterial loads, and exacerbated lung pathology. In these mice, we found higher levels of lung proinflammatory cytokines during Mtb infection, consistent with our published reports on the role of PKCδ in listeriosis and cutaneous leishmaniasis.
Remarkably, inhibition of PKCδ using a specific peptide inhibitor TatVδ1.1 (ref. ) recapitulated aggravated lung inflammation in PKCδ−/− mice during Mtb infection, revealing a direct role of this kinase in regulation of lung inflammation.
Alveolar macrophages (AMs) are essential for protection during Mtb infection in mice, and we found strikingly reduced numbers of AMs with concomitantly higher lung bacterial loads that could lead to necrosis in PKCδ−/− mice. To control enhanced bacterial burdens, activated macrophages and monocytes are recruited that perhaps explain excessive NO oxide in the PKCδ−/− lungs, in contrast to PKCδ−/− macrophages in vitro. Notably, mice deficient in AMs due to the deletion of granulocyte-macrophage colony-stimulating factor develop a disorder of accumulated surfactant lipids in the alveolar spaces of the lungs.
Despite reduced AMs in PKCδ−/− mice, we did not observe increased lipid staining in the lungs. This could be due to the increased recruitment of activated macrophages that catabolize surfactant lipids along with type II alveolar epithelial cells.
Importantly, it is feasible that due to higher bacterial burden AMs decreased in PKCδ−/− mice. Consequently, increased inflammatory cell recruitment to the lungs as a result of proinflammatory cytokines, which in turn might have decreased alveolar spaces (for gas exchange), translated in the mortality in these mice during Mtb infection. Our findings suggest that PKCδ is required for maintenance of an optimal inflammatory balance during Mtb infection that is a key factor in limiting immunopathology to host lung tissue. We infer from these findings where PKCδ ablation in mice renders them hypersusceptible to TB, and therefore it is likely that increased expression (blood) and abundance (granulomas) of this kinase reflect its role as a host factor to contain ongoing inflammation in humans.
Host lipid bodies provide an excellent nutrient source for the survival of intracellular Mtb, thereby decreasing its own metabolism that allows pathogenesisand persistence of the bacterium. The necessity of triacylglycerol for slow replication was demonstrated in a recent study where deposition of excessive triacylglycerol in Mtb bacterium slowed down its growth as opposed to a Mtb strain capable of pumping out lipids.
Reports have indicated a critical role of PKCδ in the accumulation of cholesterol in human and mouse macrophages and triacylglycerol during glucose intolerance induced by high-fat diet in PKCδ−/− mice.
Corroborating with these findings, we found that PKCδ is indeed critical for the accumulation of lipids in the lungs, macrophages, and to a lesser extent in the case of serum fatty acids following Mtb infection. The latter may not contribute much to the biological relevance owing to subtle differences. Notably, it has been shown that in steady state, absence of PKCδ is dispensable for the uptake of Ox-LDL to induce foam cell formation in murine and human macrophages.
Moreover, our observations of Mtb loads in PKCδ−/− macrophages pretreated with unsaturated, saturated fatty acids, and oxidized and native LDLs supported that lipid accumulation might not necessarily contribute to the intracellular bacterial growth in macrophages deficient for PKCδ. Recently, it was shown that increased lipids in lungs and macrophages drive the polarization of macrophages (M2) involved in fibrosis.
In PKCδ−/− mice, the decreased availability of lipids and enhanced proinflammatory cytokines might have limited tissue repair processes in the lungs. Thus, lipid accumulation can be the consequence rather than the cause of susceptibility to Mtb infection in PKCδ−/− mice. This Mtb-driven modulation of host lipids may be the means by which this highly evolved pathogen controls its replication rate in vivo. It is feasible that inability of PKCδ−/− mice to accumulate intracellular lipids hampers the ability of Mtb to undergo slow-replicative state during infection.
Intracellular Mtb can be eliminated by the induction of macrophage phagosome maturation and autophagy.
The PKC isoforms, including β and α, were reported to be important for maturation of Mtb-containing phagosomes. In contrast to PKCβ and PKCα, our findings indicated that PKCδ is dispensable for phagosome maturation and autophagy in Mtb-infected macrophages. An alternative explanation is that PKCδ, unlike other isoforms (α, β, and γ), is insensitive to calcium signaling that is important for phagosome maturation. Another isoform PKCζ has been implicated as a key factor for TLR2-ERK1/2 (Toll-like receptor 2/extracellular signal-regulated kinase 1/2)-mediated secretion of TNF in both murine and human macrophages following Mtb infection in vitro.
However, inhibition of PKCδ with rottlerin abrogated apoptosis in murine macrophages when cultured with cell-free supernatant of Mycobacterium indicus pranni (Mw).In contrast, we observed increased apoptosis in PKCδ−/− macrophages following Mtb infection. This observation strengthens accumulating evidence regarding the nonspecific actions of rottlerin as a PKCδ inhibitor.
,As we found no effect on phagosome maturation and autophagy, we probed other effector functions in which PKCδ might be involved. It is well established that within macrophages, Mtb can be successfully eradicated by oxidative (ROS, H2O2) and nitrosative (NO) killing functions.
Interestingly, IFN-γ-activated macrophages synergistically increase NO production by fivefold upon phorbol 12-myristate 13-acetate-mediated PKC activation in Mycobacterium bovis (Bacillus Calmette–Guérin (BCG))-infected macrophages
Indeed, this was confirmed in our study as the presence of PKCδ enhanced killing effector functions, whereas the absence thereof inhibited these effector responses, thereby reducing the mycobacterial killing capacity of PKCδ−/− macrophages. To our knowledge, there has been no report on a functional role for PKCδ in immunity to TB in mice and humans.
Collectively, our data revealed that PKCδ is an indicator of inflammation in both systemic and local tissue compartments during active TB disease progression in humans. Global deletion of PKCδ worsens the Mtb disease outcome in mice that exaggerated mortality with a shift toward increased bacterial burdens, exacerbated pathology, and excessive proinflammatory responses. To a lesser extent following Mtb infection, decreased lipids in lungs and macrophages of PKCδ−/− mice might further reduce the possibility for this bacterium to undergo persistence. Mechanistically, reduced killing effector functions in macrophages increased susceptibility to Mtb in the absence of PKCδ. Taken together, the onset of active human Mtb disease correlates with PKCδ expression, and conferring from our murine model, PKCδ might be a critical factor employed by the host to control exacerbation of Mtb infection.
