Research: The CSF immune response in HIV-1–associated Cryptococcal Meningitis: Macrophage activation, correlates of disease severity, and effect of antiretroviral therapy

SATVI researcher Associate Professor Tom Scriba has co-authored a research paper titled: "The CSF Immune Response in HIV-1–Associated Cryptococcal Meningitis: Macrophage Activation, Correlates of Disease Severity, and Effect of Antiretroviral Therapy" appearing in the Journal of Acquired Immune Deficiency Syndrome.
Abstract
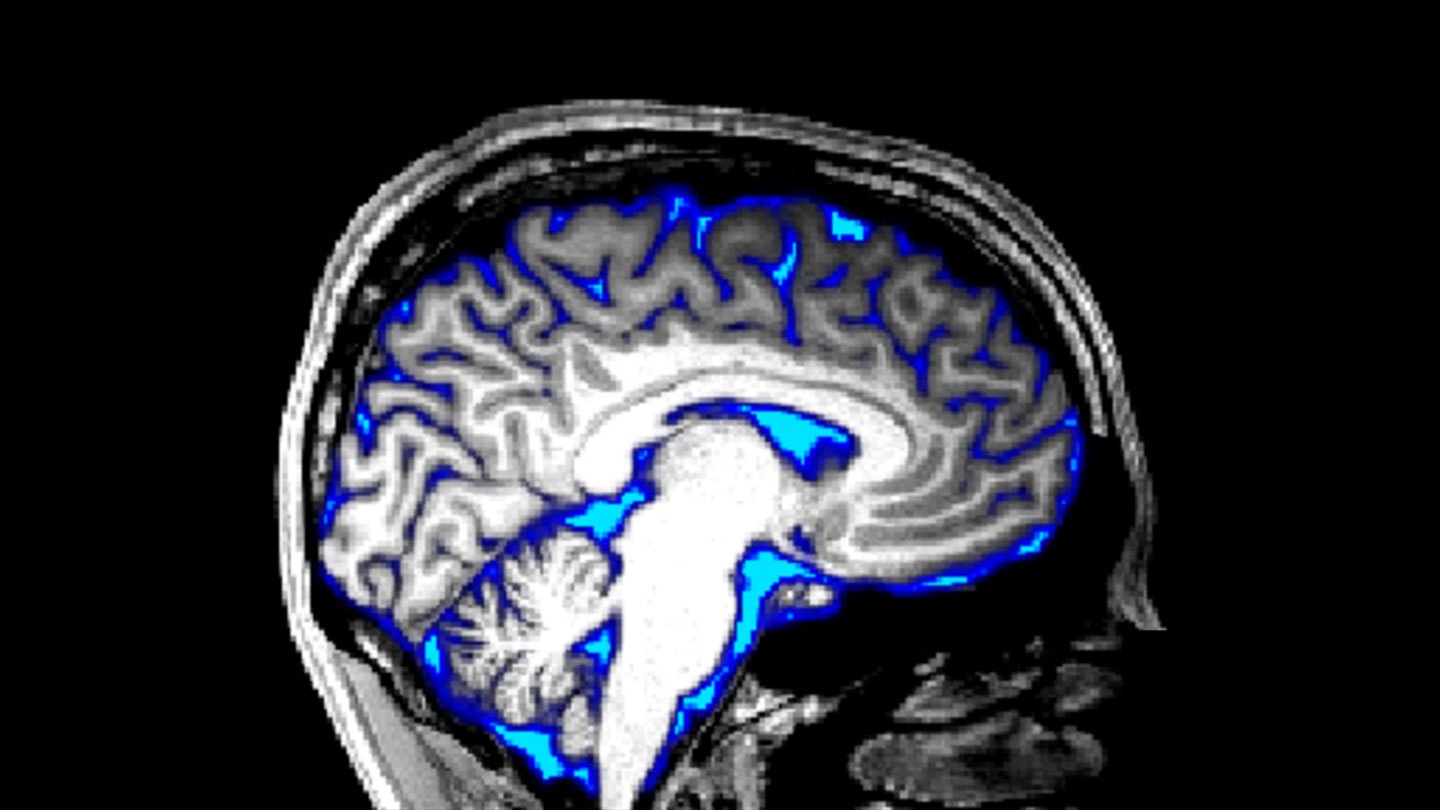
Background: Immune modulation may improve outcome in HIV-associated cryptococcal meningitis. Animal studies suggest alternatively activated macrophages are detrimental but human studies are limited. We performed a detailed assessment of the cerebrospinal fluid (CSF) immune response and examined immune correlates of disease severity and poor outcome, and the effects of antiretroviral therapy (ART).
Findings: CSF was available from 57 persons (median CD4 34/μL). CD206 (alternatively activated macrophage marker) was expressed on 54% CD14 and 35% CD14 monocyte-macrophages. High fungal burden was not associated with CD206 expression but with a paucity of CD4, CD8, and CD4CD8 T cells and lower interleukin-6, G-CSF, and interleukin-5 concentrations. High intracranial pressure (≥30 cm H2O) was associated with fewer T cells, a higher fungal burden, and larger Cryptococcus organisms. Mortality was associated with reduced interferon-gamma concentrations and CD4CD8 T cells but lost statistical significance when adjusted for multiple comparisons. Recent ART was associated with increased CSF CD4/CD8 ratio and a significantly increased macrophage expression of CD206.
