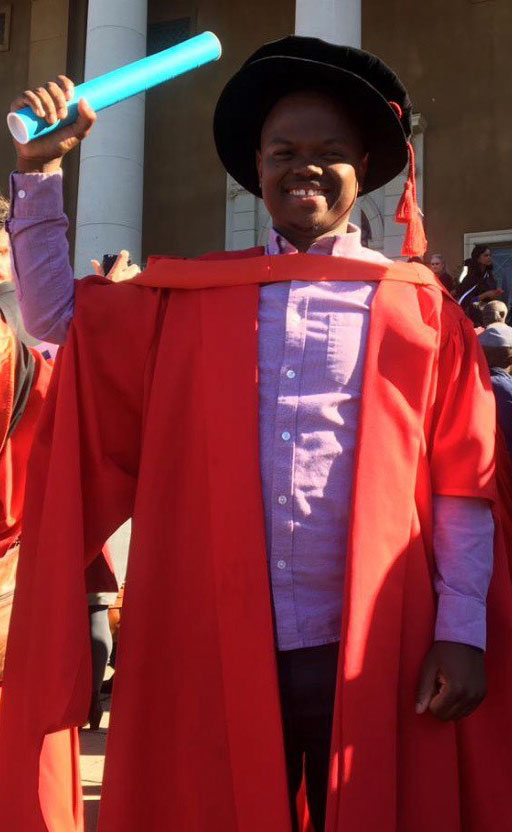
Dr Michael Zulu

Dr Zulu has now begun a Skye Foundation Postdoctoral Fellowship at the University of Surrey, Guildford, in the United Kingdom under the supervision of Dr Fernando Martinez Estrada and Prof Siamon Gordon of the Sir William Dunn School of Pathology at the University of Oxford. The postdoc study aims to identify novel markers of human decidual macrophages and Hofbauer cells throughout gestation.
Dr Zulu is currently working on a manuscript to be published from his thesis which was entitled “Characteristics of decidual macrophages and Hofbauer Cells in placentas of HIV positive women on antiretroviral therapy”. A review has already been published from the thesis in the Journal of Innate Immunity - The Elusive Role of Placental Macrophages: The Hofbauer Cell
Read Dr Michael Zulu’s PhD Thesis Abstract
Characteristics of decidual macrophages and Hofbauer Cells in placentas of HIV positive women on antiretroviral therapy
Macrophages are the most abundant immune cells at the maternal-foetal interface of term placentas. They play a role in regulating pregnancy, promoting immunological tolerance, and maintaining a homeostatic environment crucial for foetal development. Numerous studies have reported the dysregulation of maternal uterine-derived macrophages, the decidual macrophages and the foetal placental-derived macrophages, the Hofbauer Cells (HCs) in pregnancies complicated by maternal viral infections. The immune mechanisms associated with the high prevalence of adverse birth outcomes amongst HIV-1 infected women on combination antiretroviral therapy (ART) are not well characterized. In this Ph.D. dissertation, the impact of HIV-1 infection and the duration of ART exposure on the phenotype and function of decidual macrophages and HCs was studied. Birth outcomes and placenta pathologies of HIV-infected women categorized into two groups, 1). HIV-1 infected pregnant women who initiated ART during pregnancy (Initiating ART n=16); and 2). HIV-1 infected women who initiated ART before pregnancy (Stable on ART n=14) were compared. Immunohistochemical and immunofluorescence staining of formalin-fixed placental tissues from the two groups was performed to compare the expression of macrophage markers associated with inflammation (M1) and immune regulation (M2). Lastly, the Human Protein Atlas database was used to identify novel markers of decidual macrophages and HCs and their potential biomarkers of HIV-1 infection.
The expression of various M1 and M2-specific macrophage markers significantly varied between membranes of the maternal-foetal interface within the initiating and stable group. The duration of ART exposure had no effect on the expression of typical M1 and M2 macrophage markers on decidual macrophages and HCs of HIV-1 infected women who initiated a similar ART regimen before pregnancy and during pregnancy. The macrophage populations in the maternal-foetal interface co-expressed markers associated with M1 and M2 macrophage polarisation, suggesting functional plasticity of these cells. Human Coagulation Factor XIIIa1 (FXIIIa1) and Insulin-like growth factor 2 (IGF2) were identified as potential novel markers of HCs and decidual macrophages respectively, however, further validation is required. There is a paucity of data on the characteristics of decidual macrophages and Hofbauer cells in both normal and complicated pregnancies. Data presented in this dissertation suggests the possibility that HIV-infection and / the duration of ART exposure may not play an active role in dysregulating immune mechanisms associated with macrophages at the maternal-foetal interface. However, further characterization of these cells in placentas exposed to different ART regimens is required using the novel markers discovered in this Ph.D.
