Addressing the Syndemic of HIV and Suicide

Written by Morgan Watson
Background
Low- and middle-income countries (LMIC) account for nearly 80% of the global incidence rate of suicide, with the highest rates reported in Southern Africa. Not only is the region confronted with the highest suicide rate in the world, but it also carries the largest HIV burden globally. South Africa, in particular, has the highest HIV incidence, with an estimated 8.2 million people living with HIV (PWH) in 2021. Among PWH suicide is a major public health concern, yet there's a lack of research on this issue in LMIC. Suicidal ideation and behaviour (SIB) are common among PWH, who face double the risk of suicide compared to the general population. In South Africa, suicidal ideation has been reported among a quarter of people seeking HIV testing in primary care facilities. Similarly, suicidal ideation was found in 21% of newly diagnosed PWH, which increased to 29% six weeks post-diagnosis. These rates are nearly three times higher compared to the general population in South Africa, making suicide a leading cause of death among PWH. Young adults, especially those aged 25-34 are most affected. Despite these alarming statistics, the intersection of HIV and suicide remains largely unaddressed in South Africa, highlighting the urgent need for targeted interventions and research.
The syndemic of HIV and suicide demands a unique approach in low-resource settings.
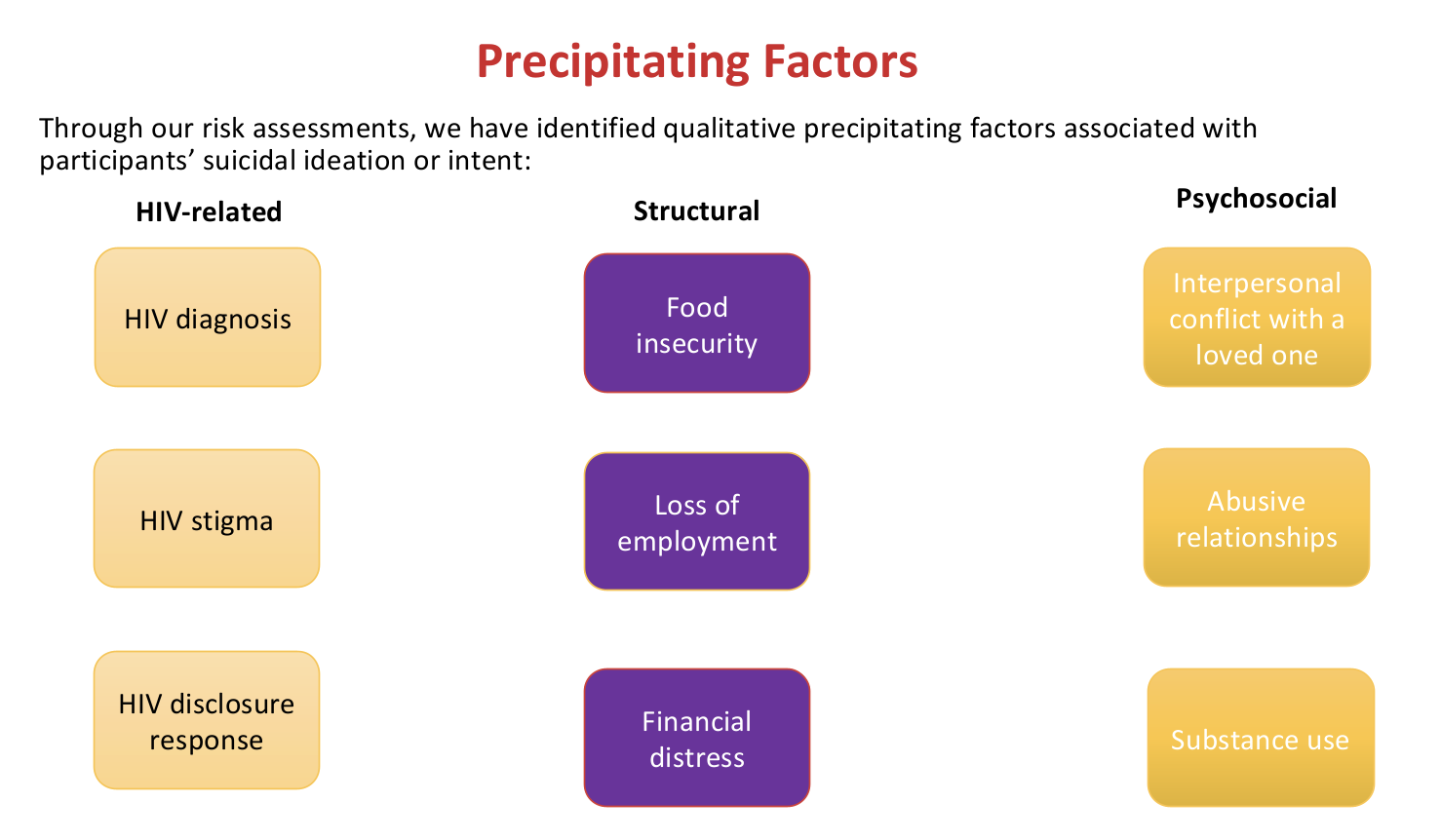
PWH face an elevated risk of suicide due to the combination of mental illness and situational stressors. Research studies highlight the urgency of addressing suicide in the context of HIV, as PWH are more prone to mental disorders like depression and anxiety. These conditions lead to delays in treatment initiation, poor HIV care engagement, and reduced life expectancy. Unlike high-income countries, where psychiatric disorders are predominant in driving suicide, low-resource settings like South Africa show that socioeconomic challenges such as unemployment and food insecurity significantly contribute to suicidal behaviour. For instance, studies in South Africa found that over half of adults who died by suicide were unemployed, and women facing food insecurity were five times more likely to report suicidal behaviour. Even when controlling for mental disorders, unemployed PWH in South Africa were nearly twice as likely to report suicidal ideation and elevated suicide risk. These findings emphasise the need for a holistic approach, considering both mental health and situational factors, in suicide prevention and intervention efforts in low-resource settings.
Where can we address the issue?
Community-based primary healthcare settings serve as crucial platforms to address suicide and enhance engagement amongst people living with HIV (PWH). Research shows that eight out of 10 individuals who die by suicide had a healthcare visit a year before their death, emphasising the significance of primary healthcare contact in suicide prevention. In South Africa, where over 80% of PWH receive HIV care in public sector facilities, this opportunity to screen for mental disorders and suicide amongst those seeking HIV care in community-based healthcare remains underutilised.
Study Aims
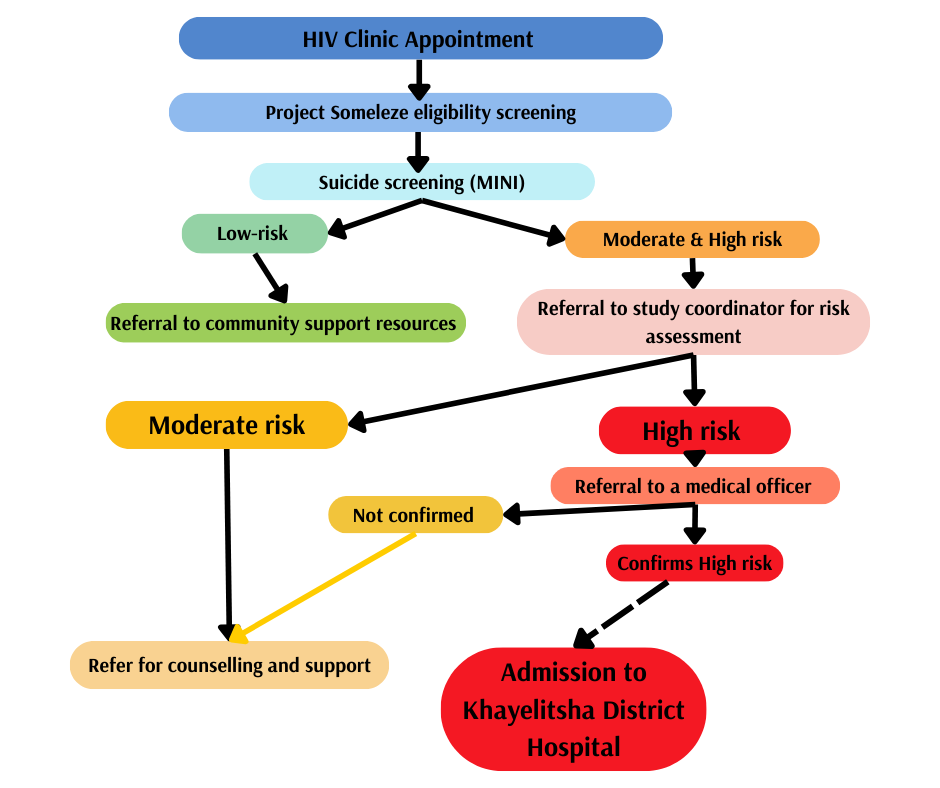
This study outlines procedures for identifying and referring HIV+ women at risk of suicide within the context of a community-based mental health clinical trial, aiming to bridge this critical gap in care.
Study method:
Data were collected as part of Project Someleze, an R01 randomised controlled trial testing the effectiveness of a coping intervention for HIV+ women with histories of sexual trauma.
Clinical staff at four primary care facilities in Khayelitsha, Cape Town referred all women initiating first-line antiretroviral therapy to study staff for eligibility screening.
Eligibility screening entailed:
- Demographic characteristics (age, pregnancy status, HIV diagnosis, ART regimen)
- 2 questions about depression (PHQ-2)
- 3 questions about intimate partner violence (WHO CTS)
- 7 questions about sexual trauma (WHO CIDI)
- 7 questions about traumatic stress symptoms (Breslau SSS-PTSD)
- 6 questions about suicide (structured screening interview)
Results
Between February 2021 and August 2023, our study involved screening 1050 HIV+ women in four community-based primary care settings. The participants, with a mean age of 32 years and an age range from 18 to 70 years, represented a diverse demographic. Amongst them, 26% (n = 269) were pregnant. The screening revealed significant mental health concerns, with 34% (n = 360) testing positive for probable Major Depressive Disorder (MDD) and 17% (n = 177) screening positive for probable Post-Traumatic Stress Disorder (PTSD). Alarming suicide-related outcomes emerged: 10.4% (n = 110) had attempted suicide in their lifetime, while 15.4% (n = 162) had experienced suicidal thoughts in the past month. Additionally, 2.9% (n = 31) were identified as high-risk for suicide and were promptly referred to appropriate care at KDH. Another 2.8% (n = 29) were deemed moderate-risk and received referrals for expedited counselling at community-based non-governmental organisations (NGOs). A considerable proportion, 15.4% (n = 162), were classified as low-risk, and they were provided with information on available community-based services, emphasising a comprehensive approach to address their needs and ensure their safety.
Conclusion
Our findings highlight the effectiveness of non-specialist practitioners in identifying and referring individuals at risk of suicide, especially in regions with limited mental health professionals. Crucial to the success of these referrals are well-established pathways and consistent staff supervision. To enhance mental health care accessibility, we advocate for the integration of mental health screening, including assessments for suicidality, within routine care at community-based clinics, presenting a distinctive opportunity for this integration. The prevalence of emotional distress amongst participants, exacerbated by various situational factors, emphasises the pressing need for comprehensive interventions. Addressing suicide in low-resource settings demands a dual focus: not only on mental health concerns such as co-occurring depression, PTSD, and substance use but also on structural challenges like unemployment, poverty, and food insecurity. By addressing both mental health and societal factors, interventions can be more effective in tackling the complex issue of suicide in these contexts.