COVID-19: Collective Experiences During Global Pandemic (Volume 3)

Mandla Majola (Community Engagement Coordinator,UCT, MCSJ) and Myrna van Pinxteren (Researcher, UCT)
Editorial Note: Mandla Majola is the community engagement coordinator for the iALARM project (www.ialarm.org.za), HIV activist, and co-founder of the Movement for Change and Social Justice (MCSJ). This past June, Mandla was diagnosed with COVID-19. After weeks of battling to overcome the illness, he was interviewed by iALARM colleague Myrna van Pinxteren and shared his story.
Down But Not Out: ‘I Need to Confront This Virus Head-On’
When Mandla started to feel poorly, he was working daily in Gugulethu and Khayelitsha. Together with Medicines Sans Frontières (MSF) and the Activist Education & Development Centre (AEDC), MCSJ set up a COVID-19 outreach campaign where they visited neighbourhoods to hand out masks, assist with COVID-19 screening, and educate residents about hygiene practices, mask wearing and social distancing. They just handed out over 15,000 masks from Umoja, a partner organisation who also trained MCSJ activists by providing sewing lessons.
“In early June, I attended several professional and personal events. I always tried to adhere to the rules, would wear a mask, keep my distance and stand close to the door. I did not want to get COVID-19, as I was worried about my mother, who is 78 years old and who I visit almost daily in Gugulethu. Everything was going well, although we would get rained on a lot during the activities, which was not ideal. On Youth Day, the 16th of June, I attended an event from Abemi (civic organisation), but really did not feel well. My chest was hurting and I felt cold, so cold.”
I was getting really depressed, but in the middle of the night, I decided that I need to confront this virus head on. I need to take my remedies so I can get better, one day at the time to fight this enemy in my body.”
Mandla went home to get some rest, but his chest remained tight and from time to time, he struggled to breath. Around the same time, his wife, Vuyiseka – also part of the outreach team in Khayelitsha – lost part of her taste and smell, one of the symptoms of COVID. “And my chest only felt more and more tight. I could hear my chest and was not able to walk far anymore.” They consulted with Dr Eric Goemaere and Dr Linda-Gail Bekker (both friends and comrades) and both got tested on the 22nd of June. “The test was hard for me, as they put a swab right into the back of your throat, which made me cough a lot.”
Besides trouble with breathing and reduced lung capacity, Mandla had other symptoms he did not expect. “I also had severe diarrhoea for three to five days, and was sweating a lot. And the breathing became worse when it was raining outside. I could feel in my chest when it would start to rain.” Mandla also had back pains, and his mother recommended he treat it with brown paper sheets to trap the heat in. “It is another traditional remedy, but it did not work for me.”
The lack of specific medication to treat COVID-19 increases people’s reliance on home remedies and herbal treatment. An interesting development, thinks Mandla. “Due the rise of biomedicine, we supressed our African way of healing. Now, the use of umhlonyana (wormwood) has become popular to treat symptoms of Corona. Most of us grew up were given umhlonyana by our moms and grandmothers to treat the flu and cold, but never really acknowledge its healing power.”
“You don’t feel dirty, but feel that whatever it is you are having is a bit scary and you should not touch anything, as it really contagious. And you feel super lonely and alone, it is a cold environment.”
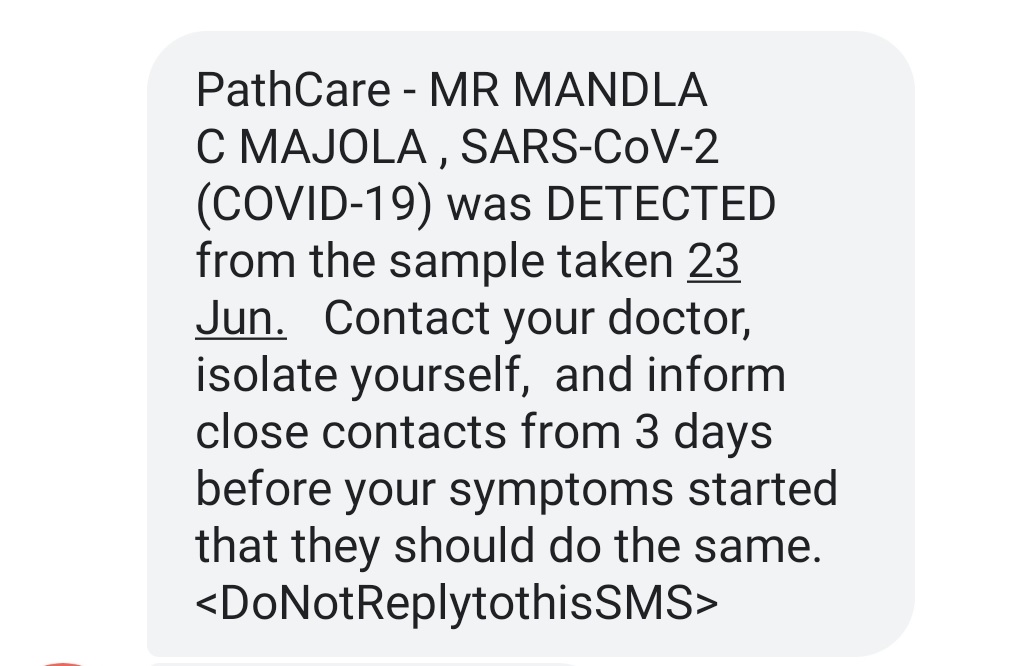
Mandla’s wife received her results via SMS first, and Mandla about 45 minutes later. After getting the news that they were COVID+, Mandla admits that he was fearful and battling to process the results mentally. “I became afraid of what was to come, as my body was not coping. I was super scared. What impact would it have on me and my family? What if I had to be admitted to hospital? And would not make it? What is going to happen with Vuyiseka, my kids? And my mother and sisters/brothers? I was getting really depressed, but in the middle of the night, I decided that I need to confront this virus head on. I need to take my remedies so I can get better, one day at the time to fight this enemy in my body.”
Despite Mandla’s fighter mentality, his symptoms became worse in the days after the diagnosis. “I was coughing so much, and my body was cold, so cold. And the sweating was also getting worse, I was changing T-shirts three times a day.” In that same week, Vuyiseka received the call that a fellow comrade from TAC, Nomandla Yako, passed away as a result from being ill from COVID-19. “I was in shock. I had known her since 2000 when she became involved in TAC. She was a dear friend and died of COVID-19. I was in shock and also scared, because I did not get better either.” Mandla and his wife again consulted Dr Linda-Gail Bekker. “She advised us to go to the hospital for an X-ray. I immediately agreed and although I was afraid and my first instinct was not to go. But through my experience with the iALARM study and my work trying to convince men to go to the clinic when they needed medical care – I know I could not be stubborn and had to listen to the experts.”
Although Mandla was convinced that the X-ray was necessary, the procedure of going to the hospital as a COVID+ patient proved challenging. First, Mandla picked up a referral letter from his GP confirming his status. When he arrived at the facility, he was sent from pillar to post. “They gave me this red pamphlet at reception and directed me to another building. But this building was closed and there was no-one answering. I commuted between the reception and the other building 4 times, walking in the rain, before a doctor assisted me. She told me that the radiology department was not informed I was coming and did not prepare for a COVID+ patient. That is why did not open for me”. When Mandla was eventually ushered to the radiology department, the gravity of the situation really dawned upon him. “It is like you land on the moon. You need to enter through a steel door and the place looks surreal.” Even though the nurses were really nice, Mandla was scared. “You don’t feel dirty, but feel that whatever it is you are having is a bit scary and you should not touch anything, as it really contagious. And you feel super lonely and alone, it is a cold environment.”
After going to the hospital, Mandla received another disturbing call. His nephew (Vuyani Majola, 23yrs) had been robbed and stabbed in Gugulethu. Listening to his crying sister, he felt extremely emotional. “I was sick, and felt terrible, but want to go to him. Vuyiseka and I drove to Gugulethu in peak traffic. I called my neighbour Phumzile Nywagi to help him getting to the clinic. When we arrived, he was okay, but I felt so powerless. I could not do anything and had to sit in the car while my wife spoke to my sister. It was a horrible day all together.”
Results of the X-ray indicated that Mandla had a mild pneumonia. He had to intensify the previously prescribed remedies and per Dr Bekker’s advice, they bought an oximeter to measure the levels of oxygen in his lungs. “My wife and I would go for short walks every day to assess my oxygen levels which, thankfully never dipped below 90%. I also took my blood pressure every morning and evening and we regularly checked my temperature.”
South Africa has overcome many crises and we will overcome COVID too. And soon I will be back in the ‘trenches’ to share my own positive COVID-19 story with everyone.”
Mandla is now recovering well from COVID-19 and his wife has already fully recovered. Reflecting back on his experience, he realises that it has been both an emotionally and physically challenging time. Despite the hardship, he is also extremely grateful for the support from his wife, his family, neighbours and colleagues. He is now reunited with his children and except of headaches, his symptoms have faded. Together with his wife, he stayed indoors for 29 days. “I have been overwhelmed by the support of others during this time. Vuyiseka was making healthy food and soups for me every day, colleagues were checking in, collaborators and funders linked to MCSJ sent messages and my manager gave me time off to recover. This has been such an important part of the healing process and I am very grateful for all the kind words.”
As an activist, Mandla was eager to share his story, as there are too little testimonies from COVID+ patients and very little information and a lack of support on how patients can address symptoms, how to use home remedies, how to access medical care, and how to deal with mental distress. “Psychologically, it was really hard. The isolation felt like an albatross around my neck. You can really find yourself longing for companionship. And people need to be prepared for that, they need to be informed about the impact of COVID-19 on their lives.”

During his time at home, Mandla reflected on the epidemic, the community response and the political strategies adopted by government. Overall, he thinks the president has been decisive and was informed by medical experts in his decision-making. “The government has been communicating clear messages based on medical evidence and international guidelines. This is so different from the leadership during the HIV epidemic, which was based on false information and denialism, which cost many lives. But I keep wondering why the ANC government is not using this leadership to address other issues that communities are battling with, including providing proper housing, sanitation and economic freedom.” Although Mandla agrees that the lockdown was effective, his experience in Gugulethu and other Khayelitsha was worrying. “For poor and working-class people, things have been rough. Some had not enough food and live from day to day. They could not afford to buy food for many weeks in a row. It worked in the wealthy suburbs, but not in the township. You still saw people going around looking for food or work to make ends meet, risking their own life and that of others in the process.”
For Mandla, COVID-19 made him realize once more that people living in informal settlements are hit hardest and need to battle both ‘third-world’ and ‘first-world’ health challenges simultaneously. “Residents in Gugulethu and other townships are more vulnerable to getting infected by TB, diarrhoea and hepatitis, due to the lack of clean water, sanitation and proper housing. At the same time, they also are susceptible to developing chronic illnesses, including diabetes, high blood pressure and hypertension.”
Mandla is also concerned about the public health services in poor communities, as clinics are already full, there is a shortage of staff and people in townships are more likely to catch COVID-19, as they are sharing toilets, taps and houses, and cannot afford to self-isolate. The early deployment of community health workers seemed promising, but in reality, was disorganised. “In the beginning, especially, the Department of Health (DOH) was struggling to trace patients in the most vulnerable settlements such as Barcelona, Europe, Vlei and Lusaka. MCSJ assisted with contact tracing and together with community health workers would deliver chronic medication for patients at home. Despite their best efforts, some patients did not receive their pills, and we needed to negotiate with clinic managers. Overall, we need to be more organised in our response.”
As an HIV activist, Mandla can draw similarities between the HIV pandemic and the COVID-19 epidemic, especially within township settings. “Again, it is the poorest communities that are hit hardest by COVID-19, similarly to HIV and TB hotspots in Cape Town. It seems that 25 years after apartheid, the lives of the poor still don’t matter and the lack of proper housing, food security and crime contributes to residents being vulnerable. Similar to HIV, health cannot be separated out from our living conditions and people from all sectors need to mobilise themselves and to keep the government accountable, that they have to invest in low-income communities.” According to Mandla, the ongoing corruption, even in these dire times, is also contributing to the issue. “People are stealing COVID grants and protective gear and our justice system fails to address this problem.”
One strategy, Mandla says, is to organise a structured community response, led by NGOs and activists, in collaboration with health care providers. “Our response to HIV was very vivid, and we also have to face this crisis head on. But we should not forget that it was also a battle to mobilise for HIV. When I joined TAC in 2001, we struggled to get people to attend our events and share their stories with the public. But we learned a lot during that time.” One of the approaches from TAC that could be replicated in the COVID-19 community response is the sharing of testimonials and positive stories, to destigmatise the disease and educate at the same time. In TAC, we had many HIV+ mothers who shared their story to stimulate others to enrol in the prevention of mother-to-child transmission (PMTCT) programmes, including Nomandla Yako. We need to encourage people who were COVID+ and have recovered to do the same. To share their experience so people are not fearful to get tested if they get symptoms.”
Although there are similarities that can be drawn between the HIV and COVID-19 responses, community mobilisation campaigns need to be structured differently, due to restrictions in movement, social distancing and absence of events. “We want to mobilise the community, but we cannot be close to each other, so we need alternative approaches. We need to collaborate with traditional and religious leaders and to support the health staff where we can. And we keep the government accountable to committing to long-term improvements and ask critical questions such as ‘why do we still have no running water in the townships, why are there not enough toilets and why is the health system overloaded?’”
In the COVID-19 response, the media has a critical role to play too, mentions Mandla. “The media needs to also share positive stories from COVID+ patients, not only report about death and the impact on the economy. These messages amplify fear in people.” Lastly, Mandla states that community outreach campaigns as organised by Medicines Sans Frontières (MSF) and MCSJ need to receive adequate funding, as they are making a real impact. “With more funds, we can mobilise ourselves better and more effectively and communities can and will come out to fight COVID-19. South Africa has overcome many crises and we will overcome COVID too. And soon I will be back in the ‘trenches’ to share my own positive COVID-19 story with everyone.”
Image Captions
Image 1: The SMS that Mandla received from PathCare confirming his COVID+ status
Image 2: Eucalyptus oil, one of the home remedies recommended to mandla to treat his chest pain
Image 3: Other home remedies used by Mandla to treat his symptoms, including peppermint drops and honey
Author Biography

Email: myrna.vanpinxteren@uct.ac.za